Maintaining normal bones during and after the menopause
During the period when women enter menopause, they will typically experience a 2-5% natural loss of bone tissue. A natural loss of bone mass up to 10-15% is seen during the first 10 years after menopause, so maintaining your bones can be a wise precaution.
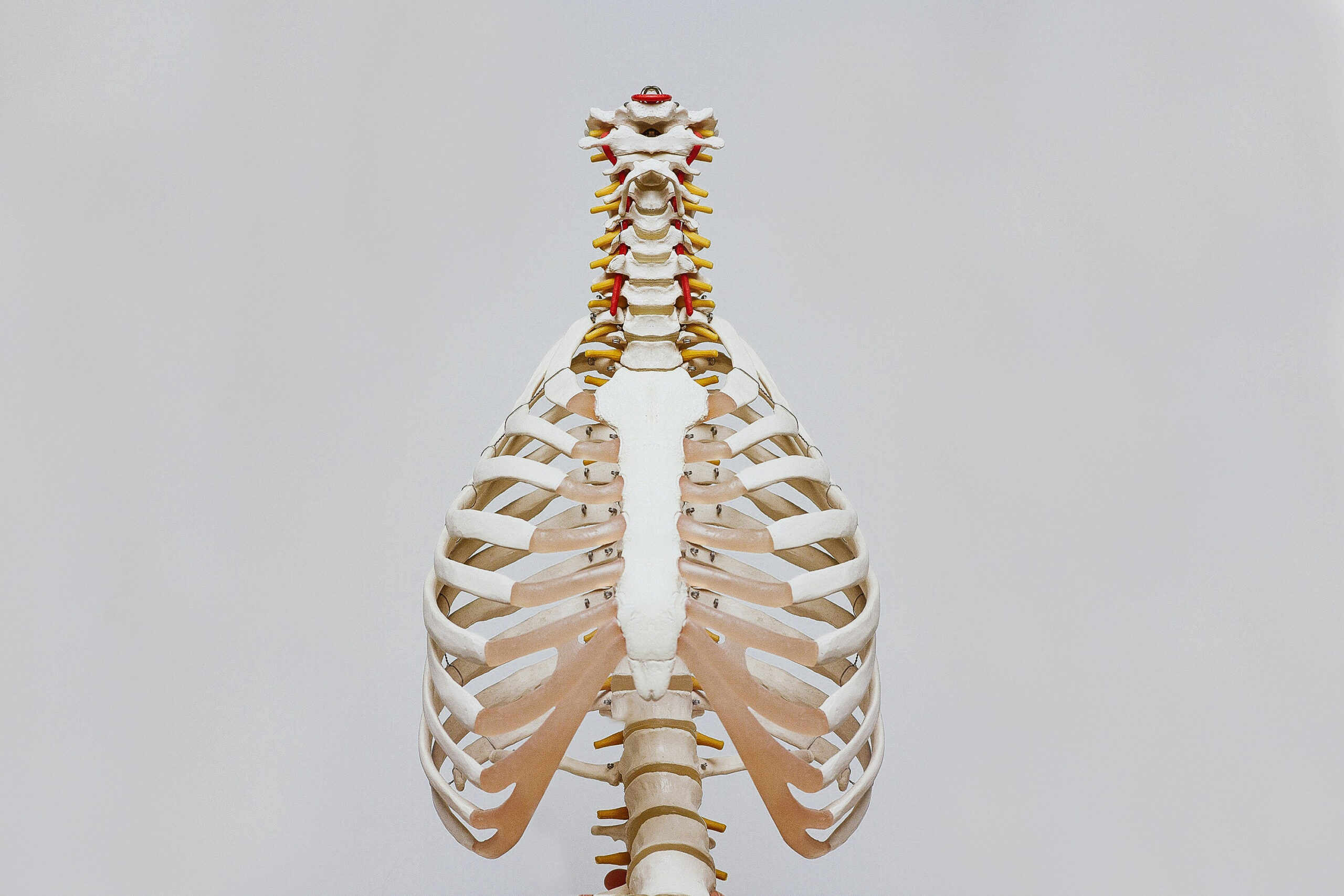
What are bones made of?
Our bodies have 206 bones, which are made of bone tissue that contains calcium. Calcium and magnesium are some of the important minerals for bones as calcium is necessary for the maintenance of normal bones. It is also necessary to consume enough vitamin D as this contributes to normal calcium absorption.
Calcium and vitamin D help reduce the bone mineral loss in post-menopausal women. Low bone mineral density is a risk factor in terms of potential bone fractures resulting from osteoporosis. A reduction in bone mineral density loss can only achieved with a daily intake from all sources of a minimum of 1,200 mg of calcium and 20 μg of vitamin D.
For people who have a specific need to maintain their bones, the Danish Veterinary and Food Administration recommends a daily intake of 800-1000 mg of calcium and 20 µg of vitamin D.
It is also important to stay physically active, avoid smoking, and otherwise eat a healthy and varied diet.
Bone tissue and bone mineral density
On average, our bones replace themselves approximately once every 10 years. Before new bone tissue can build up, old bone tissue must first be removed. Here, it is bone cells called osteoclasts that break down the bones while cells called osteoblasts build new bone tissue. This is how bones are continuously being replaced over the course of your lifetime. However, the amount of bone mass (bone tissue) and bone mineral density peaks at around the age of 30.
Bone scans – T score
Bone density can be measured by means of a DXA scan, which measures bone mineral density according to a so-called T-score scale. The T-score scale is a calculation of the standard deviation in relation to the average for young healthy people
Menopausal women
Production of the female sex hormone oestrogen decreases as women enter menopause. This is relevant as the bone-building osteoblasts are stimulated, among other things, by oestrogen production in the body. With the onset of menopause, bone mass breakdown can therefore occur at a faster rate compared to the period before menopause. Post-menopausal women will therefore (on average) have lower bone mineral density than they had before going through the menopause.
Fermented red clover, vitamins and minerals for the bones
Red clover contains plant oestrogens called phytoestrogens, which are also known as isoflavones. These agents are what make fermented red clover an attractive option during and after the menopause as their structure resembles oestrogen, the female hormone. However, unlike oestrogen, they bind mainly to the beta-oestrogen receptors in places like bones, kidneys and the brain, rather than to the alpha receptors which are mainly found in breast and ovarian tissue. When red clover juice is fermented, sugar molecules and isoflavones are split apart, and the isoflavones take aglycone form. When in this form, the isoflavones are ready to be absorbed by the body, which means that fermentation is a way to ensure increased absorption. Fermented red clover also contains natural calcium and magnesium, both of which are good for bones.
The isoflavones in red clover
Today, many red clover varieties are bred with an ever-decreasing isoflavone content. For Herrens Mark, however, the reverse is true; because the herb’s isoflavone content is what makes it an interesting plant to use. We have therefore spent a lot of time focusing on sourcing and further developing older varieties with higher isoflavone content. Herrens Mark was therefore, among other things, a participant in a large GUDP project, which ran from 2014-2018, the goal of which was to select old varieties for further enrichment, which is a process that is still ongoing at Herrens Mark to this day.